|
Healing the gut takes some time, it unfortunately doesn't happen over night. On the bright side, it's not too complicated to figure out how to start the healing process. It does take discipline to commit yourself to a healthier eating program, supplementation, and some lifestyle changes. There are simply 4 R's to follow: Remove Here is where we begin. This is truly the most important among the 4 R's. As we discussed in the past two posts, there are many factors that play a role in disrupting gut health. Those main sources being stress, unhealthy food and drink choices, and chemicals from medications.
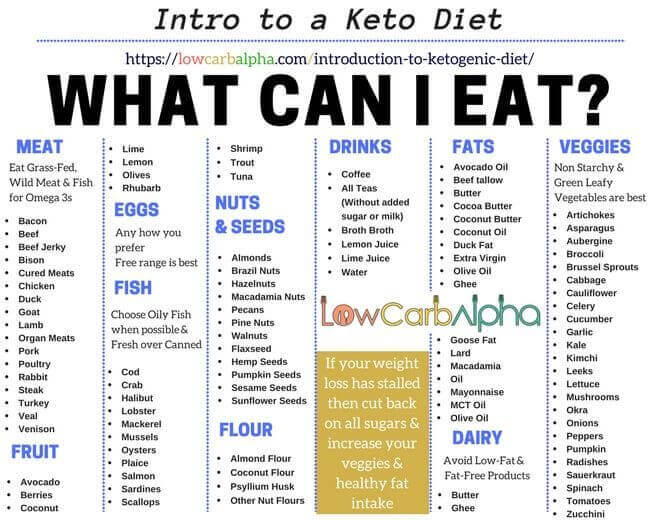
Replace How do we replace? We replace the everyday repetitive stress with time management and spending some ME time to decrease/manage the stress. Next, replace the fast food with healthy foods prepared at home (again pre-plan just a little). Replace the fake processed foods and snacks with healthy fruits, veggies, nuts, etc. Read labels and avoid poor food choices. Also replace the food sources that are highly inflammatory with alternatives. With the Gluten free trend, there are MANY options now available to help you avoid gluten. Same goes for dairy alternatives as well as eggs and nuts. As I mentioned just above, replace some of the medications with all natural supplements, whole foods, and lifestyle changes. The key here is to replace unhealthy stressors in your gut to foods that promote healing. Repair After you have made the commitment to remove and replace factors in your diet and lifestyle that are unhealthy for your gut, the next step is to repair the damage. Repairing the gut wall is a process. Thankfully the human body is amazingly resilient and SMART! This process can only happen if the stressors are all removed. It is a delicate process that involves healing the gut barrier wall, the villi, and the mucosal layer. Remember from the last blog, 70-80% of our immune system cells live within the gut.
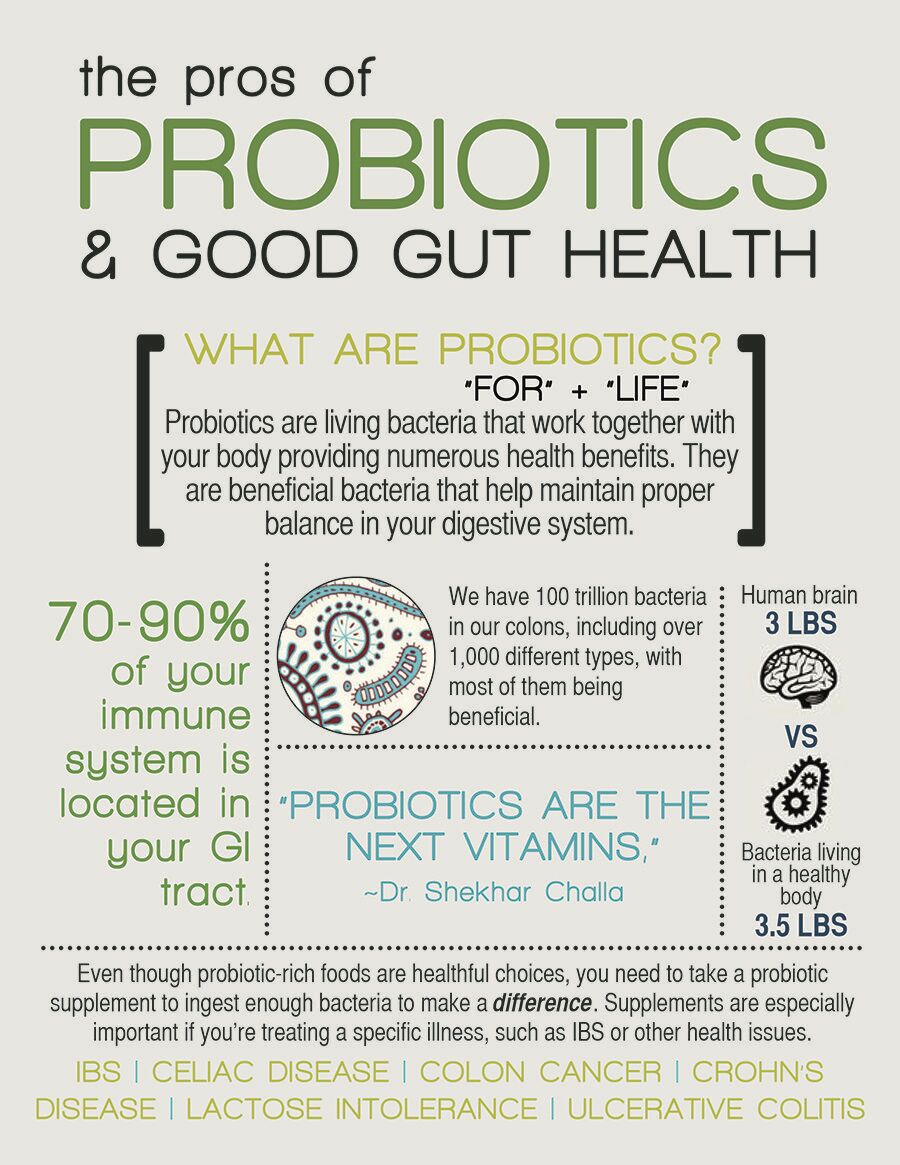
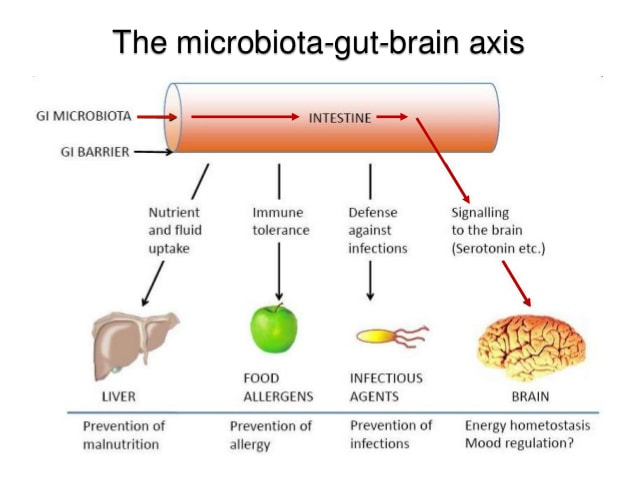
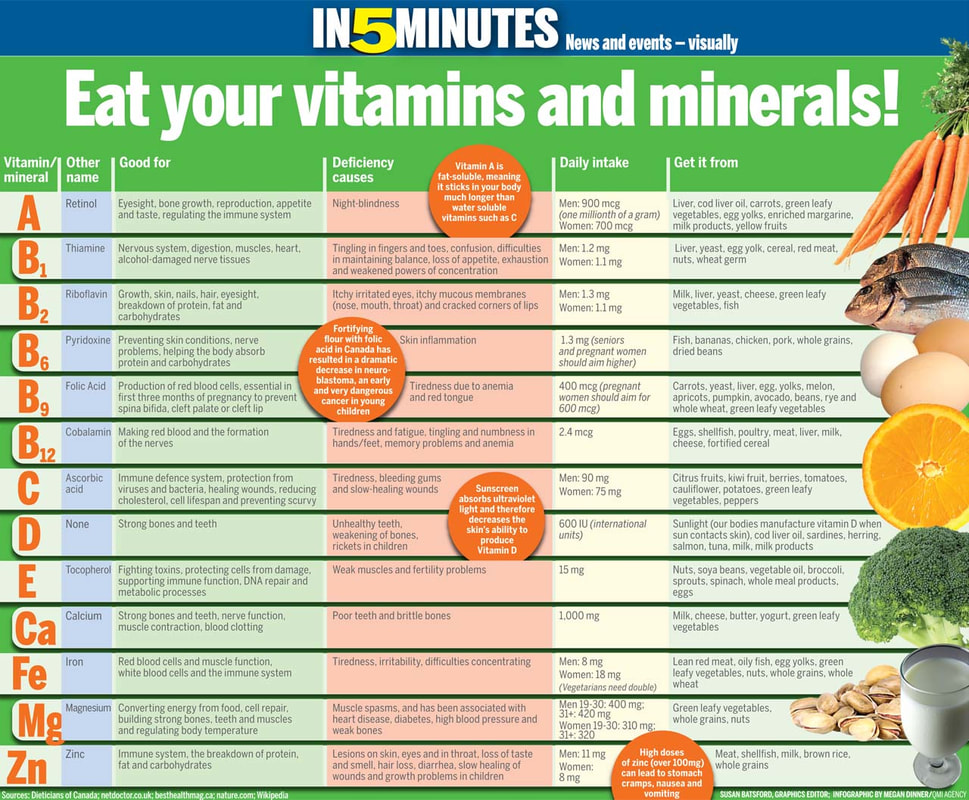
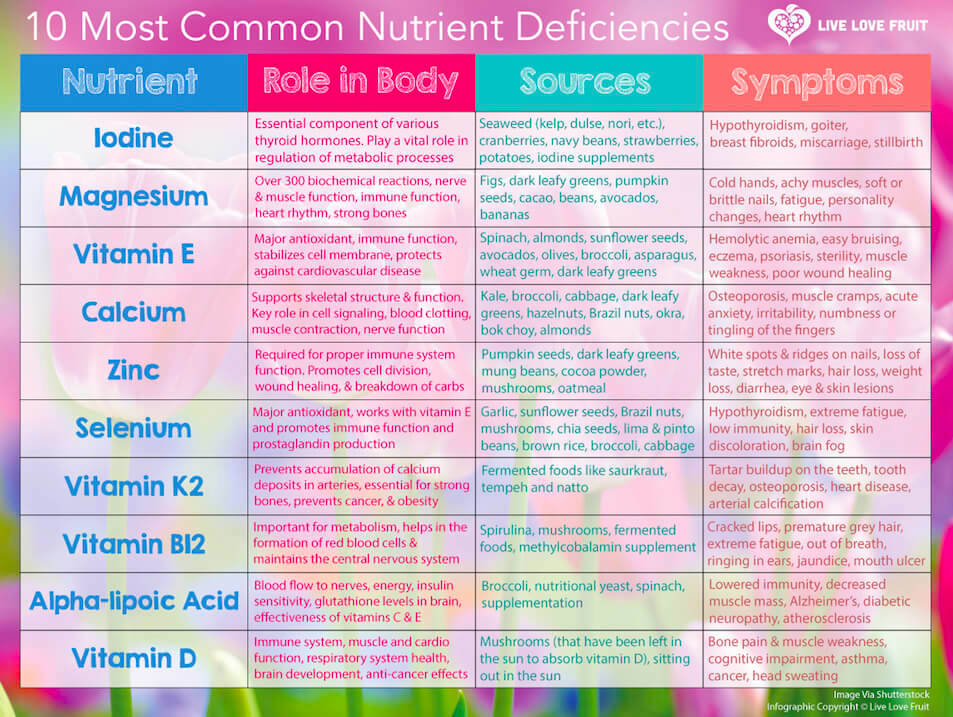
Rebalance The last step is to re-balance the GI system. While whole foods are imperative to providing nutrition for your GI health, they are typically not enough in the beginning when we are re-balancing the GI tract. The damage to the gut lining makes it difficult to utilize all of the nutrients we digest, especially if the foods are not superior quality. At this phase, reestablishing the micro-flora is paramount through probiotic support. Take a peek at the picture below Since starting to research this amazingly indepth topic on Gut Health, I have spent a lot of quality time speaking with our supplement companies to see what they officer to patients for gut health and inflammatory healing, and immune support. I was amazed at the amount of literature they were able to produce on this well studied topic. We are excited to have one of our favorite supplement reps in town next week, February 13th, to speak with not just us but also our patients and community about this interesting topic. There is so much to learn about gut health and how it's related to your overall well being. If you would like to hear more about the supplements we offer in the office for detoxification, gut repair supplements, and probiotics, please send me an email and I would be happy to help.
0 Comments
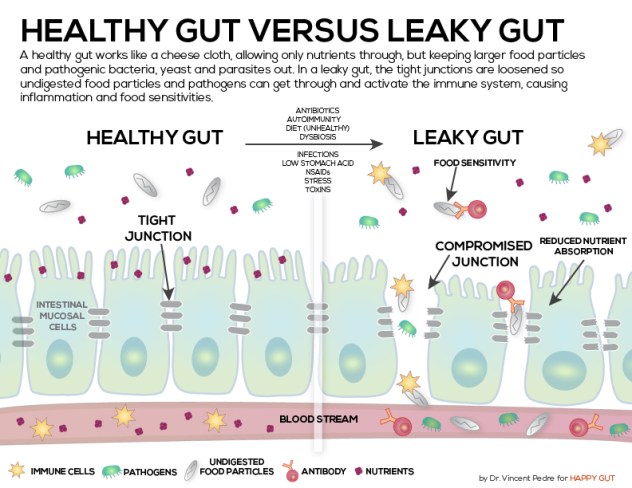
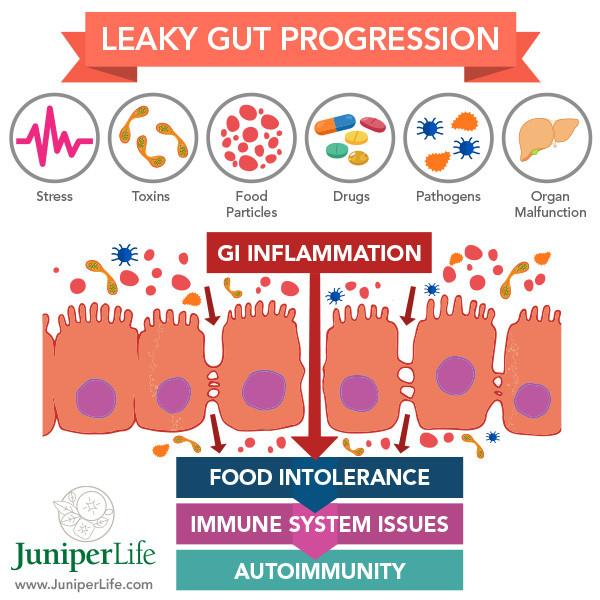
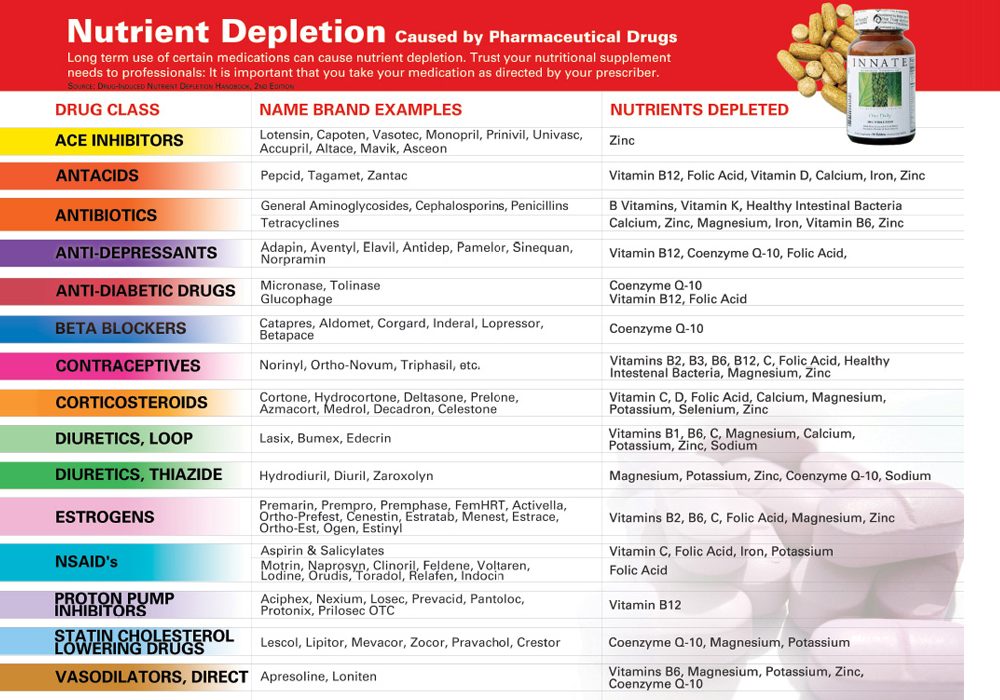
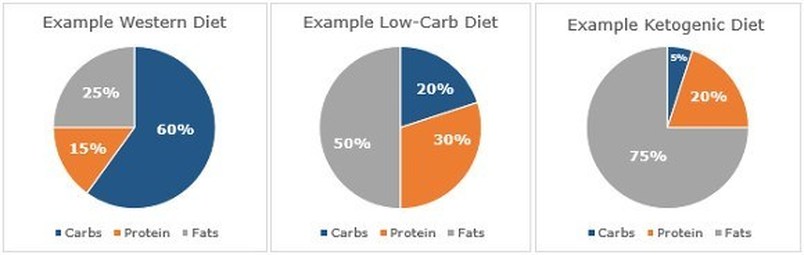
 Part I of our health gut series was an introduction into the importance of striving to keep our gut healthy. As we read, gut health is the foundation to our immune system. If we don't take care of our gut health, we disrupt our microdome, which results in damage to the intestinal barrier needed to keep foreign materials out of our blood stream. This leakage of material into our blood stream is also known as Leaky Gut. Lets go back a little bit to address the 4 top struggles that contribute to an unhealthy gut/intestinal/digestive system. 1) Stress Stress changes our hormonal balance within our bodies. With stress we find increased bowel motility and defecation while at the same time reducing gastric emptying time. Stress induced changes in the bowel motility can result in altered gut pH and nutrient absorption causing bacterial overgrowth which leads to vulnerability to pathogenic organisms. Additionally, mucosal barrier disruptions equating into an over stimulation of the immune system. 2) Diet The GI tract is exposed to 30-50 TONS of food in the average lifetime. Too many highly processed foods that are devoid of nutrients needed for health are taking over our food industry. Our diets are consisting of too many refined carbohydrates, hydrogenated fatty acids, food preservatives and food additives. Chronic poor eating places a burden on the digestive tract leading to reduced bowel transit time, sluggish detoxification, and increased inflammation. 3) Medications Drugs (over the counter or prescribed) alter the gut microbia composition. Relying on chemicals comes at a risk of damaging the gut and can be counter intuitive since these drugs have the potential to create future disease development or simply be causing the chronic issues that you are trying to treat. Common examples of medications that do a number on your gut health are:
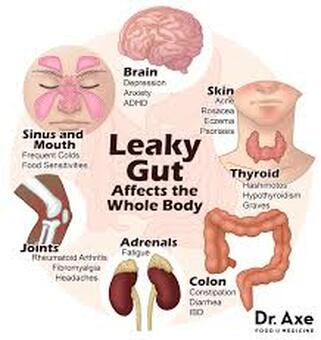
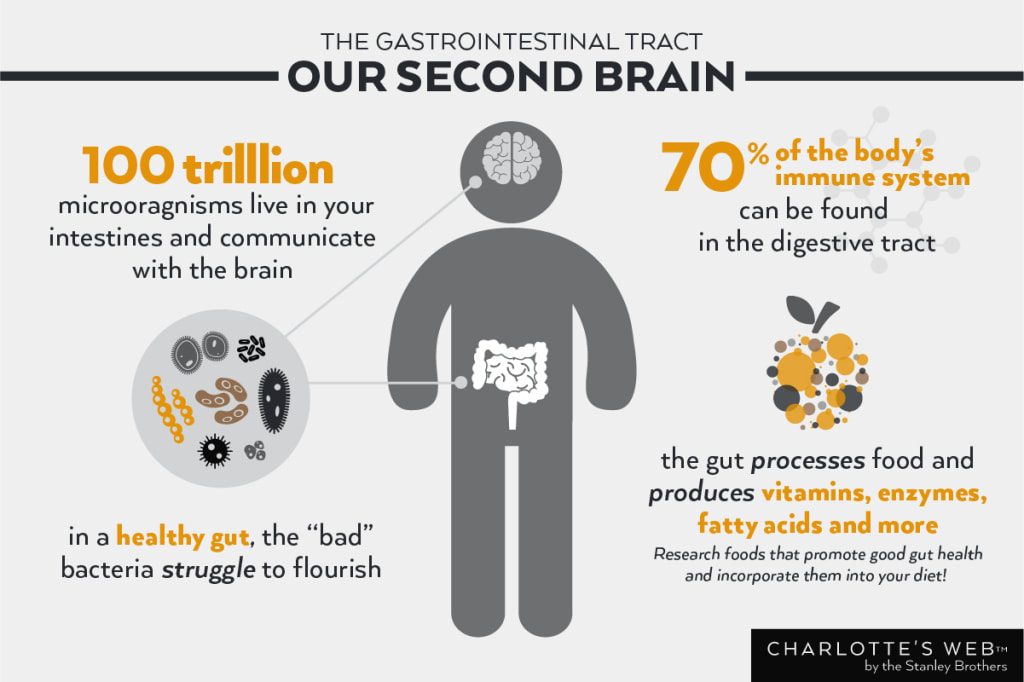
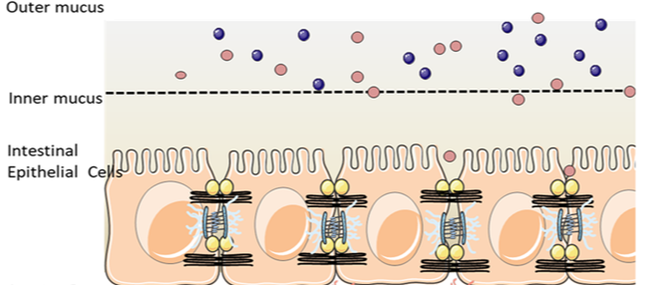
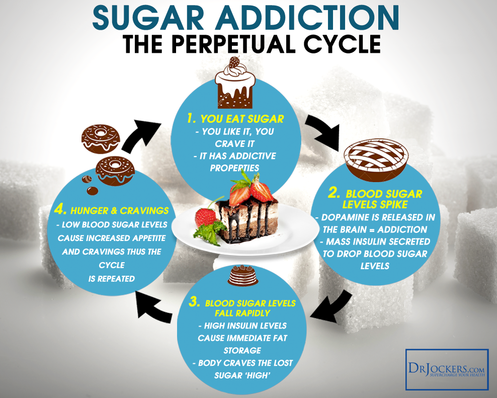
4) Food Allergies, Sensitivities, & Intolerances Any of the above can be characterized by any negative reaction to food. Food Sensitivities are non allergic immune responses to a component(s) of a food, an example is Gluten. The gliadin protein in gluten triggers an immune response causing inflammation along the inner lining of the small intestinal wall. Food Intolerance is the difficulty digesting certain foods due to a lack of proper enzymes. There is no immune response with a food intolerance, and symptoms are typically limited to diarrhea and/or vomiting. Commonly seen with eggs, milk, and gluten. Food Allergies affect 3% of our population in the IgE category. There are two types of allergic reactions from the body due to a food allergy, IgE and IgG/IgA. A little about our IgA, IgE, and IgG immune responses. IgA, IgG and IgE refer to immunoglobulins, or “antibodies.” These antibodies are part of our immune system, and are produced in response to things we come in contact with on a daily basis. Our bodies make antibodies to foreign substances like bacteria and viral cells, but can also respond to foods, dust, dander, and pollen. Antibodies help the body mount an immune system response (“fight”) against foreign invaders. IgA and IgG reactions are known as delayed response reactions, that include food sensitivities, where IgE responses are immediate and are considered a true food allergy. IgA and IgG reactions may not happen immediately, but can take hours to days to show up in your skin or intestines, and cause symptoms related to inflammation like headaches, fatigue, brain fog, or joint pain. People with food intolerance may experience digestive upset like nausea, constipation, or diarrhea, or skin itching and rashes including conditions like eczema and psoriasis. IgE immediate hypersensitivity reactions are characterized by hives and throat swelling that accompany anaphylactic reactions some people experience when exposed to certain foods. Other symptoms can include wheezing, coughing, a runny nose, vomiting, swelling of the lips or tongue, tearing or redness of the eyes, or even a weak pulse and loss of consciousness. Common foods that trigger IgE reactions are peanuts, shellfish, egg, dairy products, soy, tree nuts, wheat and fish. So how does your gut health contribute to an autoimmune disease? Autoimmune disease is on the rise in a major way. According to the National Institutes of Health (NIH), 23.5 million Americans suffer from a form of an autoimmune disease, but some think that number is actually closer to 50 million. There are at least 80 to 100 different diagnosable autoimmune diseases worldwide, and more are being studied and diagnosed every single day. We turn back to the relationship of the gut and overall health. Also the gut and our immune system, or lack thereof. Let's re-familiarize ourselves with the word below... dysbiosis /ˌdisbīˈōsəs/ an imbalance between the types of organism present in a person's natural microflora, especially that of the gut, thought to contribute to a range of conditions of ill health. Over time, having dysbiosis in your gut microbiome will eventually lead to a leaky gut. If your gut is leaky, food particles, toxins and infections can get through your intestinal lining and into your bloodstream where your immune system detects them as foreign invaders and goes on high alert, attacking them and creating inflammation. One main way inflammation occurs is that the food particles (especially gluten and casein, a protein found in dairy), toxins and infections look very similar to our own body’s cells and our immune system gets confused and accidentally attacks our own tissue, which leads to autoimmunity. This process is called molecular mimicry. Molecular mimicry is defined as the theoretical possibility that sequence similarities between foreign and self-peptides are sufficient to result in the cross-activation of autoreactive T or B cells by pathogen-derived peptides. (*This is google worthy on a snowy day if you are more interested in autoimmune origins.) It’s a cycle that works like this: altered gut microbiome or dysbiosis => leaky gut => food, toxins and infections into bloodstream => immune system attacks body due to molecular mimicry => autoimmune disease. In March of 2018, Yale University did a study on the gut bacteria in humans and mice. They discovered that certain bacteria in the gut (E. gallinarum) is able to trans-locate outside of the gut into the lymph nodes, liver, and spleen. This bacteria attacked tissues outside of the gut and initiated the production of auto-antibodies and inflammation. It was a theory that these foreign substances that leaked out of the gut and trans-located also invaded the incorrect cell space by Molecular Mimicry. 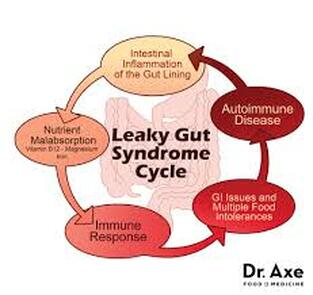 Dr. Axe that helps to simplify and describe the cycle we start to struggle with when health of our gut starts to decline. Symptoms This is a list of symptoms that are the most common with people struggling with poor gut health. It's truly exciting to think that we can start healing many health problems simply with diet. Going back to eating whole foods is understandably not the easiest when McDonald's has your food ready in 2 minutes with barely any clean up, BUT 5, 10, 20+ years from now when you are living with a slew of medical problems and feel miserable every single day you are guaranteed to look back and regret taking the extra time and effort to prevent your problems. Next week we will discuss taking those first steps to heal your gut. I will try to help simplify your plans for eating healthier and simply making better choices for yourself and your family. “A huge proportion of your immune system is actually in your GI tract,” says Dan Peterson, assistant professor of pathology at the Johns Hopkins University School of Medicine.Welcome to our series on gut health. This is one of those topics that is overwhelmingly MASSIVE and hard to even know where to start. You have likely heard or maybe even researched a little for yourself, on the topic of gut health. Maybe you know that probiotics are pretty good for you, you are just not sure why. I'm just going to scratch the surface a little bit today on gut health, then I will dig deeper for you in the subsequent weeks to come. What is the gut Microbiome? “Just like any other environment on the planet, our bodies have their own ecosystems -- made up of 100 trillion microorganisms, or microbes, that live in and on our bodies," says Rachael Buck, PhD, Abbott's lead research scientist and resident gut health expert. "These include bacteria, fungi, viruses and other types of tiny organisms. It’s so large in fact, that the genes of microbes outnumber our body’s genes by 100 to 1." The Gut Microbiome Explained (© 2019 Abbott) When it comes to the microbiome, the large intestine (or, the colon) receives the most attention because it contains the highest concentration and greatest diversity of microbes in the entire body. The large intestine is lined with a layer of mucus and the microbes that live there form a gut biofilm. The biofilm contains an array of different microbes that carry out different tasks in your body and also work together to keep you healthy.What’s even more fascinating is that each and every person has a unique make-up of microbes. What determines the different types of microbes in a person is a result of ones genes, age, gender, diet, hygiene, and even the climate you live in and your occupation. In fact, studies show that the gut microbiome affects everything from pain, mood, sleep and stress, to how our bodies use the food we eat and how we fight off infection.
|
AuthorsDr. MJ Wegmann, Archives
July 2023
Categories
All
|










 RSS Feed
RSS Feed